ORA SYSTEM® with VerifEye+TM Technology
Lock on to your refractive target
Intraoperative guidance
The ORA SYSTEM® draws from over 2 million cases and counting1
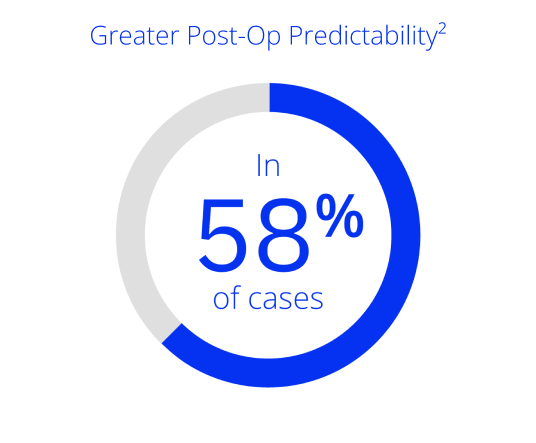
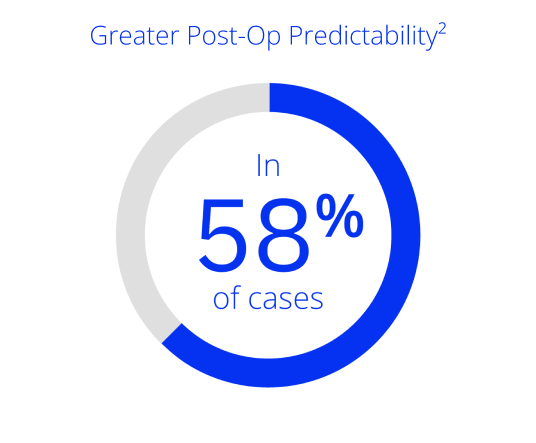
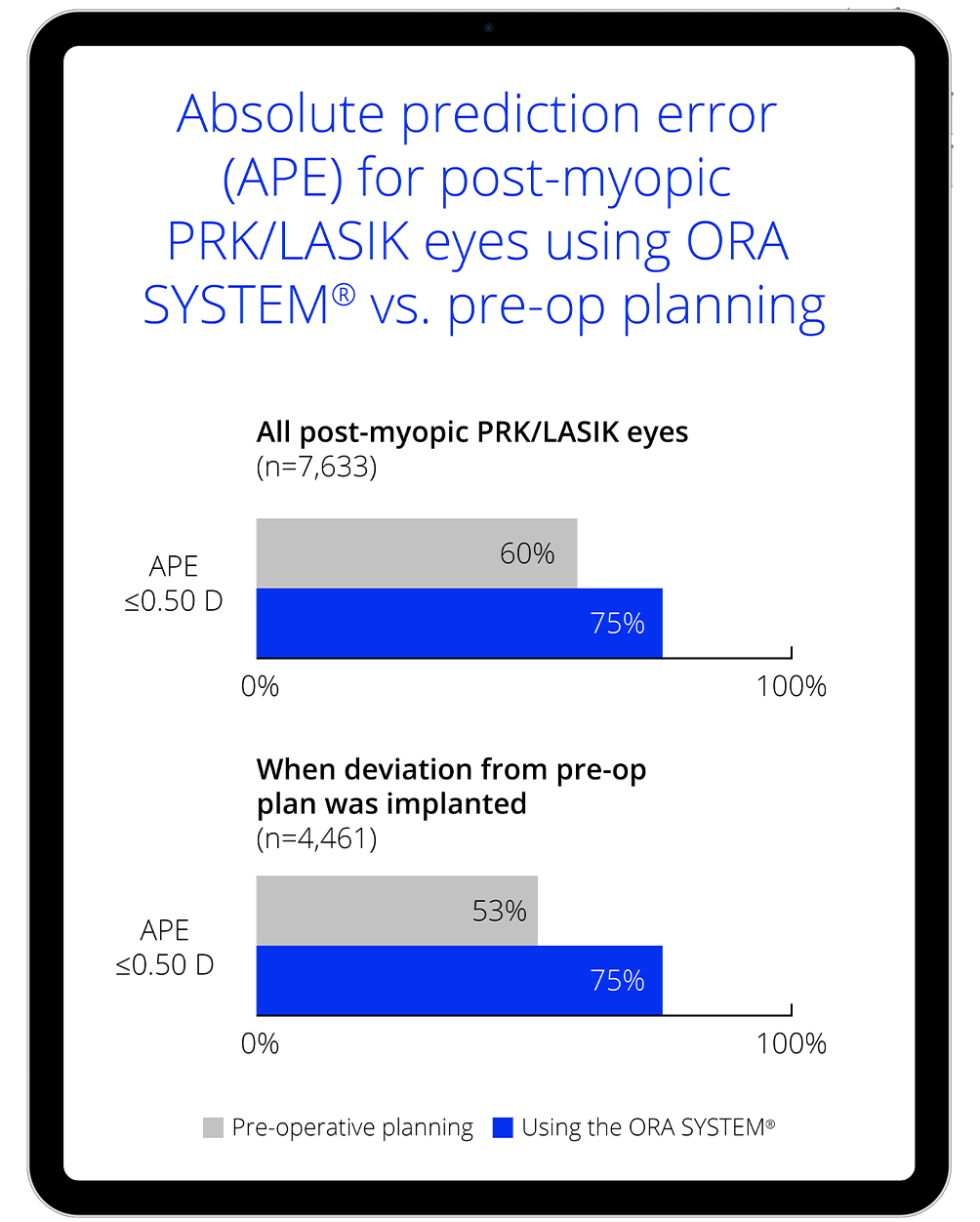
The ORA SYSTEM® influenced surgeons to change the IOL power, resulting in fewer refractive surprises* for post-myopic PRK/LASIK eyes vs. pre-op planning in 58% for cases.
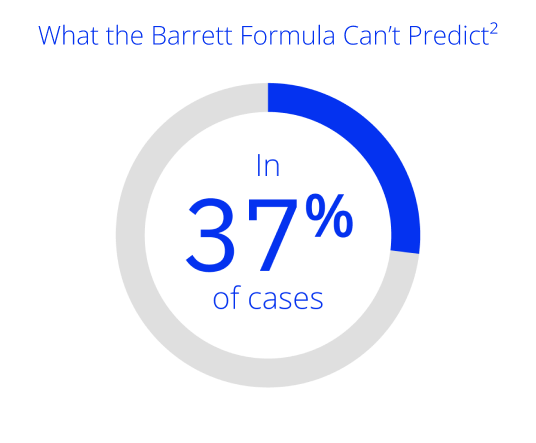
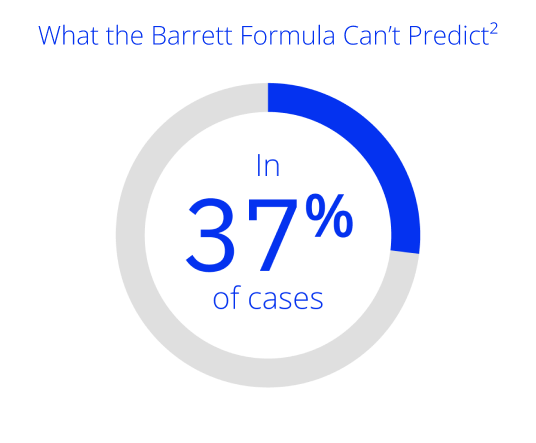
The ORA SYSTEM® influenced surgeons to change the IOL power, leading to improved refractive outcomes* in all eyes vs. the Barrett formula in 37% of cases.
*For the purpose of this analysis, a refractive outcome that deviated by greater than 0.50 D from target was considered a refractive surprise.
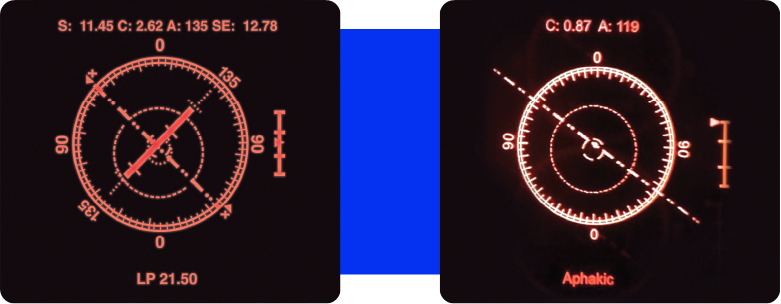
ORA SYSTEM® powered by AnalyzOR™ Technology is the one and only intraoperative aberrometer to bring precise, real-time confirmation to every case.
- Continuous assessment of your patient's eye throughout the procedure
- Customized surgical planning
- IOL sphere, cylinder and alignment suggestions
- Dynamic variable optimization
- Robust reporting with AnalyzOR™ Technology
Real-time, streaming information in your ocular with VerifEye+™ Technology
Optimize refractive correction and see when a different lens power selection may be better for your patients.
Optimize your outcomes
ORA SYSTEM® Technology provides real-time measurements of the patient’s eye during surgery, allowing you to confirm you’ve hit your refractive target in the moment. When you can validate your calculations before you implant the IOL, you’re adding a critical layer of assurance and accuracy to your procedures.2-13
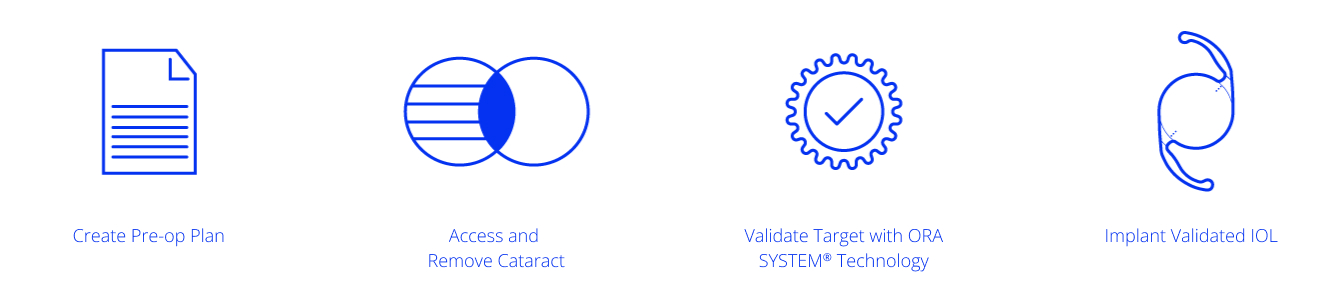
Predictable outcomes2
Streaming data allows you to position toric IOLs within 1 degree of accuracy, letting you reinforce your pre-op formulas with real-time refractive guidance.
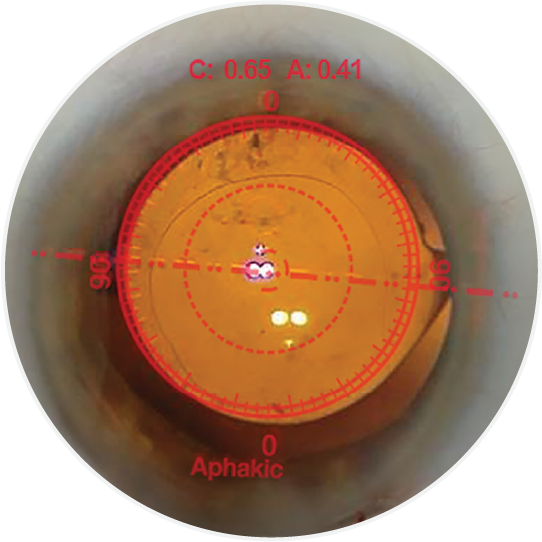
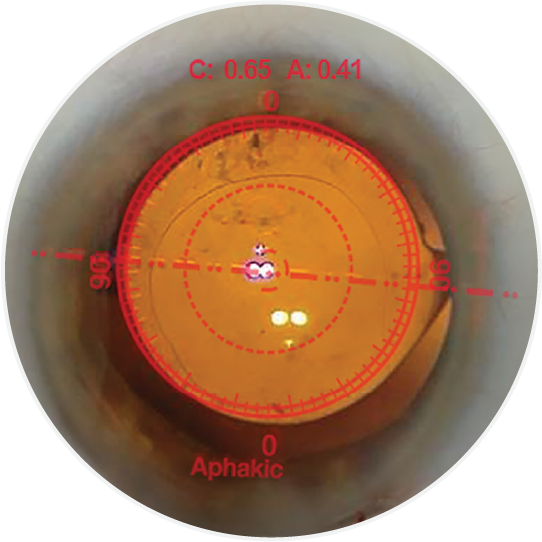
Experience convenient visual guidance for precise toric IOL rotation.


Assess refractive impact of lens options during implantation.
ORA SYSTEM® has been clinically proven to improve refractive outcomes at the time of cataract surgery in many patient groups:

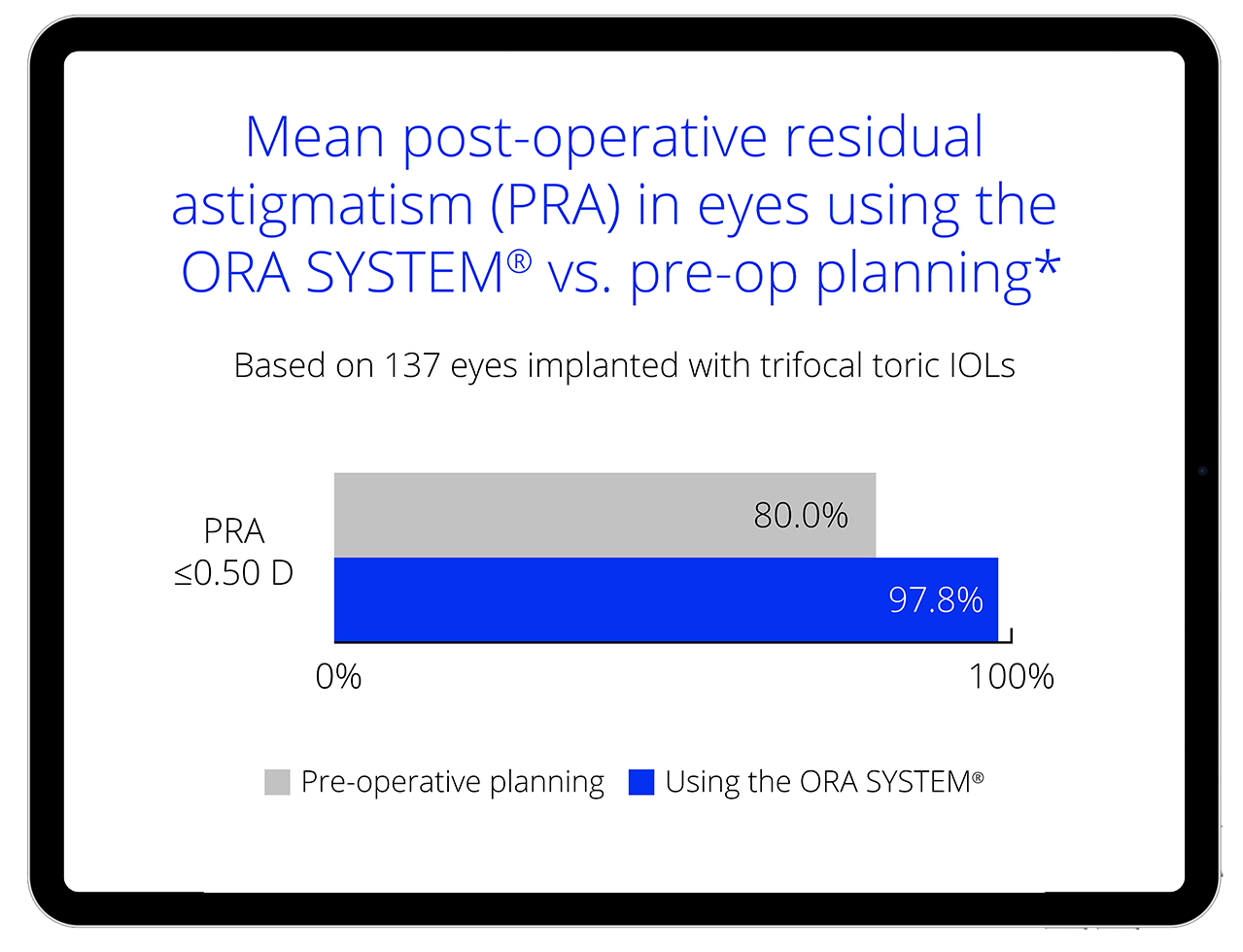
Astigmatism
In 5 studies that measured residual astigmatism, ORA SYSTEM® outperformed pre-op evaluation and planning in all, reducing mean diopters of residual astigmatism by 19% to 32%3-7*

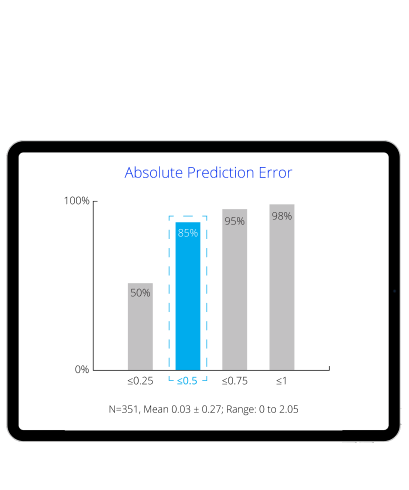
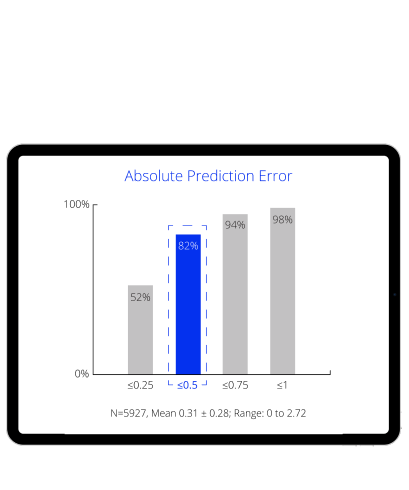
Prior refractive surgery
ORA SYSTEM® showed lower or significantly lower MAE in eyes with LASIK, PRK or RK, versus different preoperative devices and several common formulas8-10

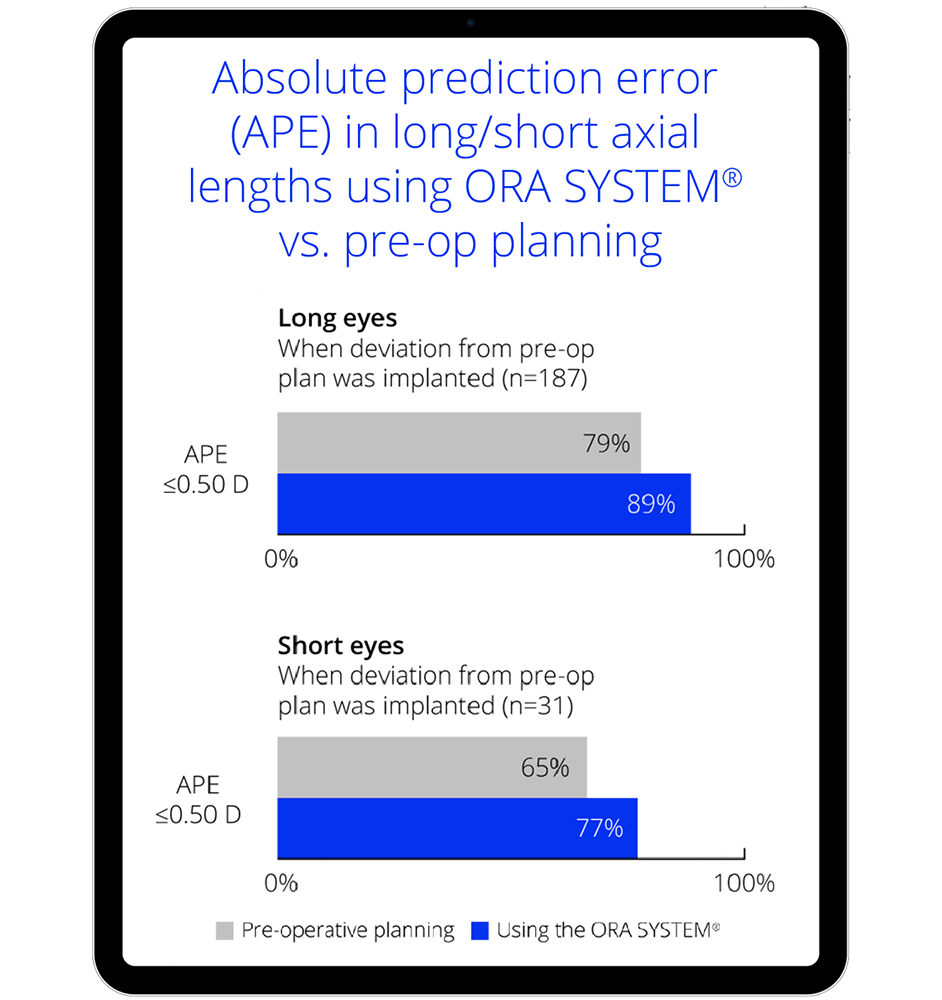
Short eyes
ORA SYSTEM® demonstrated low mean numerical error (MNE) statistically equivalent to zero, comparable to many conventional formulas11†
Long eyes
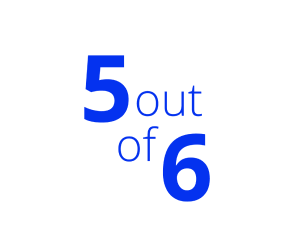
ORA SYSTEM® showed significantly lower MNE compared with 5 out of 6 conventional formulas tested (P<0.001), including Barrett Universal II and Hill-RBF formulas12
* Literature review performed January 2004 - September 2019.
† Including Hoffer Q, Holladay 2, Barrett Universal II, and Hill-RBF formulas in short eyes.
Proven accuracy
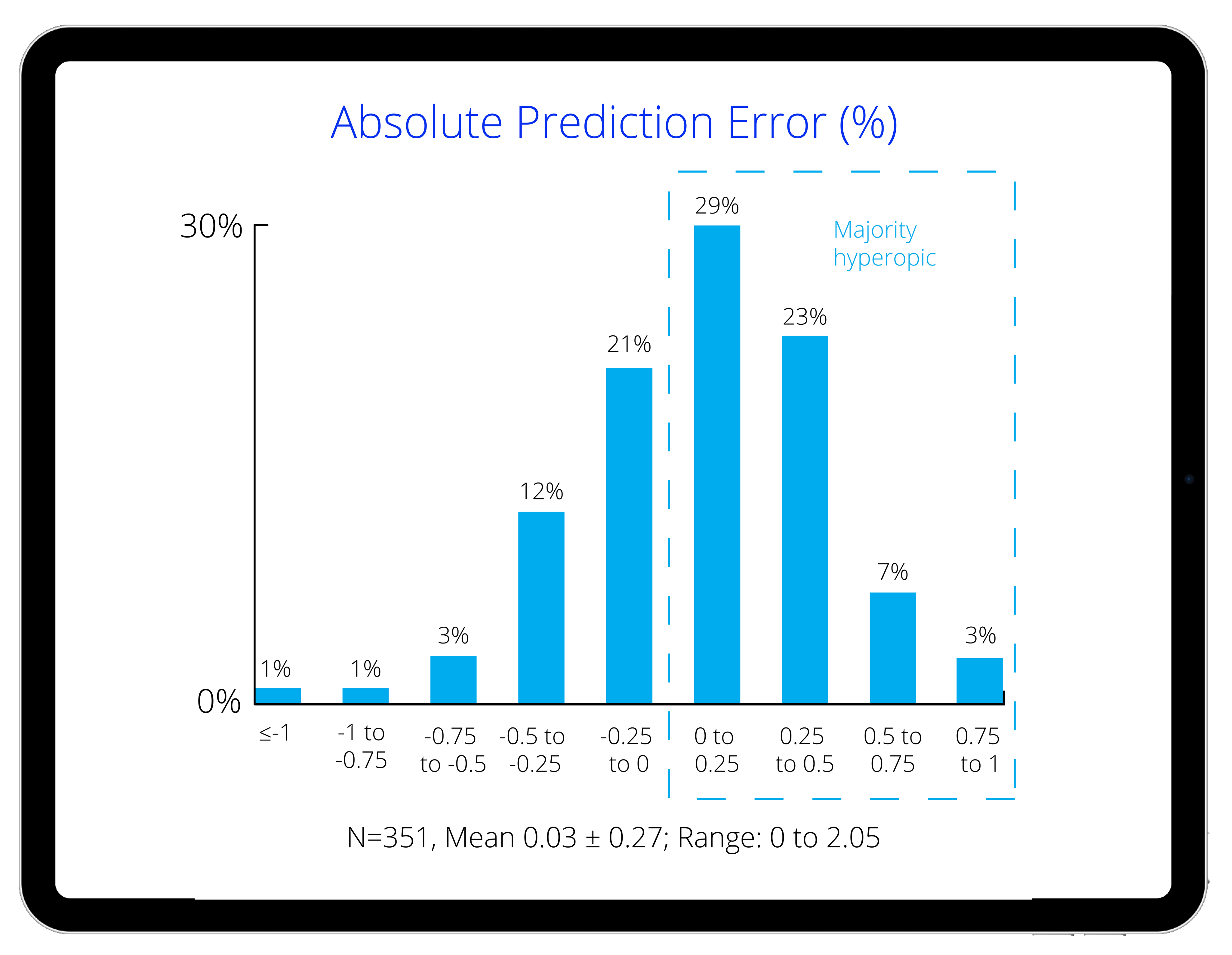
Improve your ATIOL refractive outcomes13
Now with data for presbyopia-mitigating IOLs, you can expect more from your treatment plans and your results.
*Back-calculations were performed to simulate the refractive error had the preoperative planned cylinder power and axis of placement been used. D, diopter; IOL, intraocular lens; MRSE, manifest refraction spherical equivalent; ORA, Optiwave Refractive Analysis; PRA, postoperative residual astigmatism; SD, standard deviation
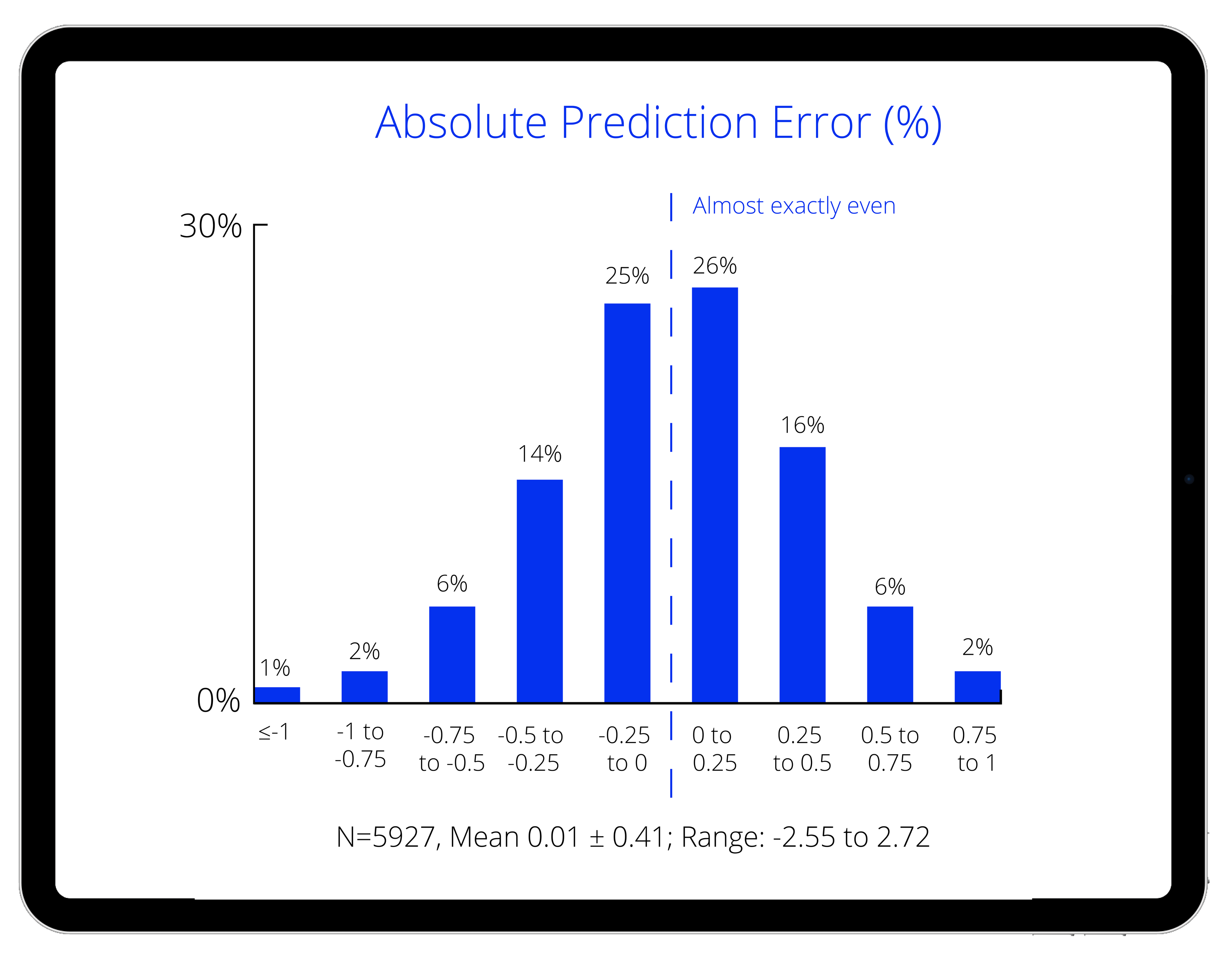
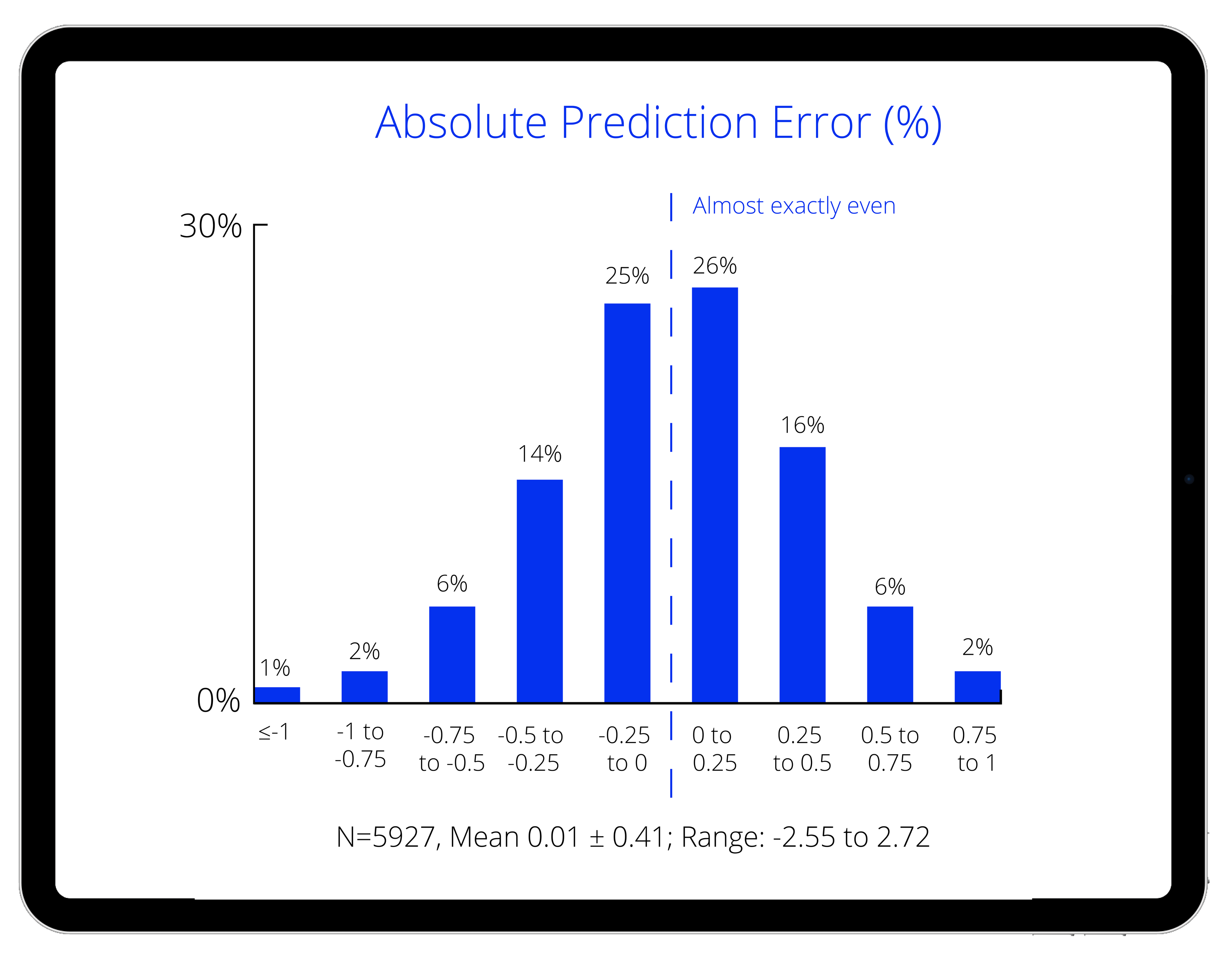
Make adjustments and avoid refractive surprises across axial lengths2*
More reliable outcomes, for both long and short eyes.
*For the purpose of this analysis, a refractive outcome that deviated by greater than 0.50 D from target was considered a refractive surprise.
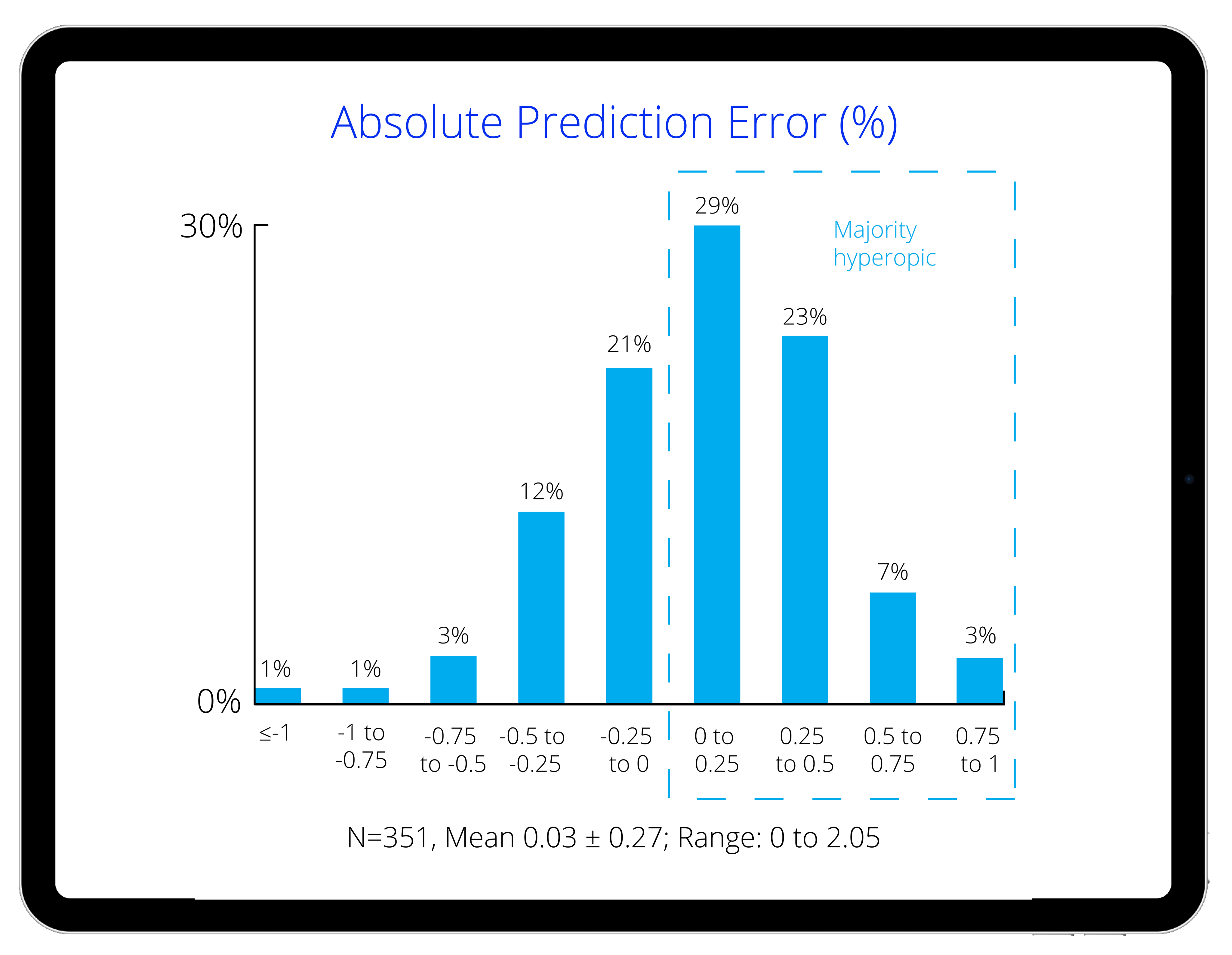
Post-myopic PRK/LASIK patients, with greater post-op predictability2
The ORA SYSTEM® influenced surgeons to change the IOL power in 58% of cases, resulting in fewer refractive surprises.*
*For the purpose of this analysis, a refractive outcome that deviated by greater than 0.50 D from target was considered a refractive surprise.


Personalization is Power
AnalyzOR™ Technology stores, tracks, and analyzes your outcomes for
personal and global trends, so that data from each procedure can enhance
the next, to improve the rate of outcomes within 0.50 D of target.6
Identify personal trends and compare against global data with ease
AnalyzORTM Technology can help you hit your refractive target
AnalyzORTM Technology can help you identify your trends
Accuracy tracking
Optimize your formulas based on current outcomes data from over 2 million real-world cases, and counting.1


Alcon Experience Academy
A non-promotional training and education resource for eye care professionals.
ORA SYSTEM® Technology – HCP Important Product Information
CAUTION:
Federal (USA) law restricts this device to the sale by or on the order of a physician.
INDICATIONS:
Federal (USA) law restricts this device to the sale by or on the order of a physician.
INTENDED USE:
The ORA SYSTEM® technology utilizes wavefront aberrometry data to measure and analyze the refractive power of the eye (i.e. sphere, cylinder, and axis measurements) to support cataract surgical procedures.
WARNINGS AND PRECAUTIONS:
The following conditions may make it difficult to obtain accurate readings using the ORA SYSTEM® technology:
- Patients having progressive retinal pathology such as diabetic retinopathy, macular degeneration, or any other pathology that the physician deems would interfere with patient fixation;
- Patients having corneal pathology such as Fuchs’, EBMD, keratoconus, advanced pterygium impairing the cornea, or any other pathology that the physician deems would interfere with the measurement process;
- Patients for which the preoperative regimen includes residual viscous substances left on the corneal surface such as lidocaine gel or viscoelastics;
- Visually significant media opacity, such as prominent floaters or asteroid hyalosis, will either limit or prohibit the measurement process; or
- Patients having received retro or peribulbar block or any other treatment that impairs their ability to visualize the fixation light.
- Use of iris hooks during an ORA SYSTEM® technology image capture will yield inaccurate measurements.
In addition:
- Significant central corneal irregularities resulting in higher order aberrations might yield inaccurate refractive measurements.
- Post refractive keratectomy eyes might yield inaccurate refractive measurement.
- The safety and effectiveness of using the data from the ORA SYSTEM® have not been established for determining treatments involving higher order aberrations of the eye such as coma and spherical aberrations.
- ORA SYSTEM® technology is intended for use by qualified health personnel only.
- Improper use of this device may result in exposure to dangerous voltage or hazardous laser-like radiation exposure. DO NOT OPERATE the ORA SYSTEM® in the presence of flammable anesthetics or volatile solvents such as alcohol or benzene, or in locations that present an explosion hazard.
ATTENTION:
Refer to the ORA SYSTEM® Operator’s Manual for a complete description of proper use and maintenance, as well as a complete list of contraindications, warnings and precautions.
1. Alcon Data on File. 2021
2. Chen M, Reinsbach M, Wilbanks ND et al. Utilizing intraoperative aberrometry and digital eye tracking to develop a novel nomogram for manual astigmatic keratotomy to effectively decrease mild astigmatism during cataract surgery. Taiwan J Ophthalmol. 2019;9(1):27-32.
3. Hatch KM, Woodcock EC, Talamo JH. Intraocular lens power selection and positioning with and without intraoperative aberrometry. J Refract Surg. 2015;31(4):237-242.
4. Packer M. Effect of intraoperative aberrometry on the rate of postoperative enhancement: Retrospective study. J Cataract Refract Surg. 2010;36(5):747-755.
5. Woodcock MG, Lehmann R, Cionni RJ, et al. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser: one-month results. J Cataract Refract Surg. 2016;42:817-825.
6. Davison JA, Makari S, Potvin R. Clinically relevant differences in the selection of toric intraocular lens power in normal eyes: preoperative measurement vs. intraoperative aberrometry. Clin Ophthalmol. 2019;13:913-920.
7. Canto AP, Chhadva P, Cabot F et al. Comparison of IOL power calculation methods and intraoperative wavefront aberrometer in eyes after refractive surgery. J Refract Surg. 2013;29(7):484-489.
8. Ianchulev T, Hoffer KJ, Yoo SH et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology. 2014;121(1):56-60.
9. Fram NR, Masket S, Wang L. Comparison of intraoperative aberrometry, OCT-based IOL formula, Haigis-L, and Masket formulae for IOL power calculation after laser vision correction. i. 2015;122(6):1096-1101.
10. Sudhakar S, Hill DC, King TS, et al. Intraoperative aberrometry versus preoperative biometry for intraocular lens power selection in short eyes. J Cataract Refract Surg. 2019;45(6):719-724.
11. Hill DC, et al. Intraoperative aberrometry versus preoperative biometry for intraocular lens power selection in axial myopia. J Cataract Refract Surg. 2017;43:505-510.
12. Blaylock JF & Hall B. Astigmatic results of a diffractive trifocal toric IOL following intraoperative aberrometry guidance. Clin Ophthalmol. 2020;14:4373-4378.